1801006200 - SHORT CASE
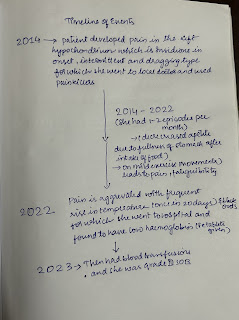
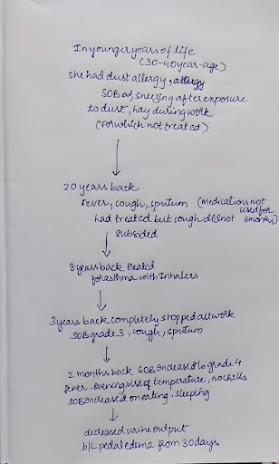
1801006200 - SHORT CASE THIS IS AN ONLINE E LOG BOOK TO DISCUSS OUR PATIENT'S DE - IDENTIFIED HEALTH DATA SHARED AFTER TAKING HIS / HER /GUARDIAN'S SIGNED INFORMED CONSENT .HERE WE DISCUSS OUR INDIVIDUAL PATIENT'S PROBLEMS THROUGH SERIES OF INPUTS FROM AVAILABLE GLOBAL ONLINE COMMUNITY OF EXPERTS WITH AN AIM TO SOLVE THOSE CLINICAL PROBLEMS WITH COLLECTIVE CURRENT BEST EVIDENCE BASED INPUT. This E blog also reflects my patient centered online learning portfolio and your valuable inputs on the comment box is welcome. I have been given this case to solve in an attempt to understand the topic of " patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with diagnosis and treatment plan A 23 YEAR OLD FEMALE CAME TO OPD CHIEF COMPLAINTS - Left abdominal pain since 1 year HISTORY OF PRESENTING ILL NESS - Patient was apparently asymptomatic 9 years back